I just finished reading Dr. Atul Gawande's recent essay "
Personal Best" in
The New Yorker. Continuing with his theme of performance improvement in health care, Dr. Gawande explores the value of coaching in medicine. Citing examples in sports, musical performance, and public education, Dr. Gawande makes a clear distinction between the coaching model and the traditional pedagogic model. In the traditional pedagogic model the assumption is that there is a point where an individual has enough expertise to not only determine what his or her weaknesses are but also how to approach improving on those weaknesses. The coaching model does not hold this assumption and says that an additional expert perspective allows individuals to continue to improve when their own capacity for self-perfection has reached a limit.
As a medical student, I am always intrigued by Dr. Gawande's ideas for the field I have chosen. However, this particular article has struck another chord with me in another field that has been an interest of mine for a long time: education. In the article, Dr. Gawande writes about the Kansas Coaching Project that advocates coaching to improve teacher performance over policy-making that punishes under-performing teachers and school systems. The project appears to have merit and would probably benefit many school systems.
The concept of peer-coaching in education is not really new to me. As a tutor in various subjects over the years, I have had been lucky to work in some well organized programs that either hold regular staff meetings, assign personal supervisors, or both to discuss ideas on what is and is not working in tutoring sessions. Like the Kansas Coaching Project, I could hear about aspects of my tutoring that could use improvement, even if it was minor. Sometimes, I would play coach, too, and share some of my own creative strategies for getting students to understand material.
As a tutor, I believe I was more receptive to an outside perspective because I knew I was not a professional teacher. I have never taken any kind of education class in my life and most of my ideas for tutoring are derived from a self-analytic experience as a student. I would imagine that professional educators might not always be receptive to the idea of someone coaching them. As Dr. Gawande notes, recognized experts who have years of training and experience behind them might feel that the days of testing and being observed are far behind them.
But what about teachers in higher education, which consists almost exclusively of those with PhD's (and in the case of medical schools like mine, many teachers have at least an MD)? Unless their field of study is actually education, college and graduate school professors usually have received little or no formal training in education. Again, another assumption is made that is akin to the first assumption of the traditional pedagogic model. It is believed that after years of experience and training as an expert in their respective fields, professors are capable of finding the best ways to impart knowledge to others.
But ask any of my fellow classmates at my medical school and you will find out that this is definitely not true of all professors. In fact, there will probably be a general consensus on which professors students feel are good and which ones are bad. What makes the difference between these kinds of teachers? There are many factors. Perhaps one day I will catalog them as I explore my interest in medical education but, for now, let me give you a for instance. The following is from a paper on cognitive load theory in health professions education by Jeroen J G van Merrienboer and John Sweller:

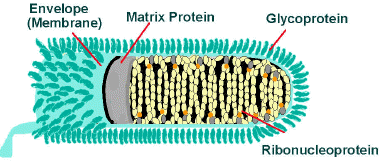
This could be any slide in an anatomy lecture on the lungs. On the left is a non-integrated format with lots of text, some of which is redundant. To the student there is a lot of visual information to take in and couple that with a professor who is speaking while this slide is displayed and the student can become overwhelmed as their attention is split between the professor and the slide. The extraneous cognitive load needs to be decreased. Note that the slide on the right still imparts the same information about the branching of the lung bronchi but reduces the amount of unnecessary description. The visual information is reduced and the students can allot their attention to the auditory information coming from the lecturer and not feel overloaded.
One thing that students may notice about a bad professor is that he or she may consistently use slides like the one on the left and their lectures become unproductive. It seems so minor a thing, the design of lecture slides. Arguments could be made that the attention should be devoted to the lecturer while actually in the lecture. But in the end, it is only natural for the mind to give attention to new stimuli that is presented to us.
If coaching can improve the performance of teachers in public education by pointing out things like ineffective slide design, those in higher education can certainly benefit from the same. Right now, students and teachers in higher education are enculturated into what I call an academic machismo. The prevailing belief is that if you just power through a lecturer's shortcomings and memorize what is on the slide over and over again like doing reps with free weights then you can be an intellectual strongman.
As a tutor, I have given many talks with students that this is not necessarily effective. Students need to be encouraged to think about how they learn and what are the best strategies to employ for themselves. Teachers need to remember what it was like to be a student and think about what kind of lectures they enjoyed. I will concede that this not always easy for teachers. In their mind, the concepts students may struggle with are commonplace for them. But this is what coaching could do for professors at universities or medical schools. In the end, it will be the students who benefit and that does not seem so lofty a goal for any institution.
Works Cited
Gawande A. "Personal Best." The New Yorker. 3 October 2011.
van Merrienboer JJG, Sweller J. Cognitive load theory in health professions education: design principles and strategies. Medical Education. 2010; 44: 85-93.
Afterword
To the writers of the articles I have discussed should, you ever come across my lowly blog, I hope you will view my inclusion of your work as admiration of the deepest form and a free promotion of all your work.